
Peripheral artery disease (PAD) is common. About one out of every 20 people in the U.S. over the age of 50 has this condition, which reduces blood flow to the limbs, usually the legs. Yet, there are many differences in how and when people seek treatment and in their outcomes.
Most often, PAD is caused by atherosclerosis, in which plaque builds up in the arteries causing them to become narrower, reducing the supply of blood flow. Atherosclerosis is not limited to the limbs, and can accumulate in any blood vessel, raising the risk of dangerous outcomes such as heart attack or stroke. Serious forms of PAD like critical limb ischemia can lead to amputation if untreated.
As common as it is, PAD doesn’t cause symptoms in as many as 65% of people. Among those who do have symptoms, the most common is claudication, or pain and cramping while walking. Other symptoms can include:
Coldness in one arm or leg
Discoloration of the affected limb
Numbness or weakness in the affected limb
Wounds that don’t heal
Reducing disparities begins with understanding each patient’s unique situation, including non-medical factors like their socioeconomic status, to determine the best treatment for every individual.
Disparities in PAD
Studies have shown that women are at 30% higher risk of developing PAD than men. Additionally, women are more likely to be diagnosed with PAD that is more severe. Research into risk shows that 30% of Black men and 27% of Black women will develop PAD in their lifetime, compared to 22% of Hispanic men and women and 19% of White men and women. While differences in risk factors such as smoking, diabetes, and high blood pressure rates may contribute to these differences, disparities remain even when these factors are considered.
Complications from PAD treatment such as infection, bleeding, and blood clots are more common among Black people. Due to PAD, people who live in rural areas and have lower socioeconomic status are more likely to have an amputation. Studies have shown that Black patients have a greater likelihood of dying from PAD than White patients, too.
There are many reasons for these differences. Patients with lower financial means are less likely to be able to seek care due to concerns such as transportation or inability to take paid leave from work. These patients are more likely to have comorbid conditions such as diabetes, high blood pressure, and high cholesterol. Because PAD is linked to other conditions and lifestyle choices like smoking, treating it alone can have negative effects. To make things more complicated, studies have shown that fewer Black patients know that PAD can lead to amputation, and Black patients are more likely to have PAD with no symptoms. When first-line treatments are less effective as the condition gets worse, this may delay seeking treatment. Treating the patient, not the disease.
The providers at MedStar Health are committed to creating the most effective treatment plans for each individual patient’s circumstances. The reasons why plaque builds up in the arteries of the limbs are not always obvious. Some factors that can increase the risk include:
A family history of PAD, heart disease, or stroke
Race
Being over age 50
Having diabetes, high blood pressure, or high cholesterol
BMI
cigarette use The Limb Salvage Center at MedStar Georgetown University Hospital is committed to saving as many limbs as possible. To accomplish this, podiatrists, plastic surgeons, orthopedic specialists, and more work we work closely with patients to discuss their lifestyle, goals, financial situation, worries, and support system. Considering a patient’s home life can help determine which treatment pathway will offer the best chance of a positive outcome.
There are also many services available through MedStar Health that can help. In order to provide free care to registered individuals, we collaborate with Catholic Charities. Prescriptions can be more affordable with the help of cost assistance programs. As a not-for-profit health system, our Financial Assistance Policy is designed to help our neighbors get the care they need regardless of their income. Disparities can be reduced with the help of these programs and others. There are many effective treatments for PAD. Lifestyle adjustments may be able to treat PAD on occasion. Making healthy changes can help relieve symptoms and stop PAD from getting worse. This means adopting a healthy diet, participating in supervised exercise therapy, and stopping smoking. Our experts work together to support patients through these important changes.
Medications can be helpful in treating PAD. Collaborating with our colleagues, we recommend the right drugs to manage blood pressure, cholesterol, and diabetes.
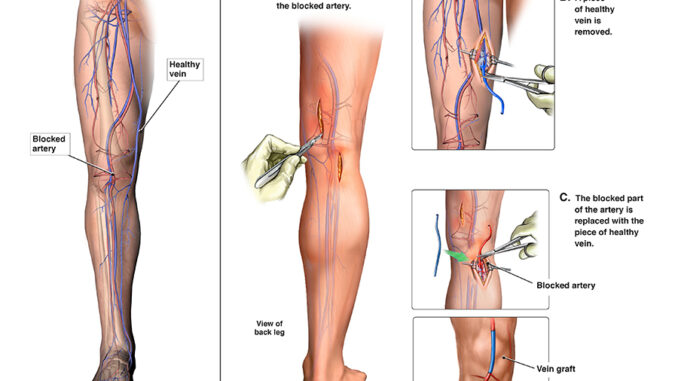
In severe cases of PAD, surgery to restore blood flow may be an option to possibly avoid amputation. Minimally invasive procedures can open the arteries, and bypass surgery can reroute blood flow.
enhancing outcomes for all parties. To help overcome barriers to care, I recommend that patients and doctors hold honest, open conversations. We want to help all patients be their healthiest, so we want you to mention when something doesn’t feel right. The more information we have, the better we can customize your care.
Even if you’re seeing your cardiologist, don’t hesitate to bring up something unusual with your toenail. It could be a sign of a condition such as PAD.
PAD is a complicated condition with many factors at play. The first steps toward equitable outcomes happen when diagnosis is early, and patients and providers work together to design a personalized, realistic treatment plan.
